Electrical Station 4.2 LAB
Electrical Systems in Health
The Heart and Cardiac Arrest

Note: You MUST complete one of the scheduled CPR certification classes before you complete this lab station.
Lab Goal: To check for and calculate pulse and breathing rates, to correctly perform Hands Only CPR or full CPR if equipment is available, and to demonstrate the correct use of an Automated External Defibrillator (AED).
Lab Materials Required: Heart model, adult CPR manikin, Practi-Shield CPR Training Face Shield, Practi-TRAINER Universal AED Trainer, calculator, pencil, and Answer Sheet. (All provided)
Objectives for Experiment:
- Explain how the heart works through electric impulses.
- Identify the four heart chambers, each of the great vessels, and explain how blood flows through the heart and lungs.
- Correctly calculate pulse and breathing rates.
- Identify ways to know when someone is in cardiac arrest.
- Demonstrate how to perform Hands Only CPR and use an AED.
- Demonstrate how to perform full CPR using a face shield and an AED.
- Correctly define the terms in bold from the introduction.
- Correctly answer application questions relating to the lab experiment.
Prerequisite knowledge: Minimum 6th grade reading level. All instructions provided.
Process Summary: At this station you will…
- Work with a heart model and try to identify all four chambers and the great vessels
- Identify where each heart chamber pumps blood to, and where each great vessel delivers blood
- Review the medical vocabulary and read instructions on how to perform a pulse check and breathing check, and how to calculate rates for each
- Practice taking a pulse and breathing rate on three people, and calculate heart rate and breathing rate for each person
- Learn and practice how to correctly perform Hands Only CPR and use a trainer to practice using an AED
- Learn and practice how to correctly perform full CPR with a face shield and use a trainer to practice using an AED.
Applied Health Terminology: Like many professions, the medical field has its own vocabulary. We have created flashcards to help you learn some of the vocabulary related to joints and movement that was used in this lesson.
You can find these flashcards on the computer at the site below.
Instructions to site:
- Click on the link below.
https://quizlet.com/86476027/electrical-station-42-cpr-and-aed-use-flash-cards/
- Then click on the “Flashcards” button in the upper left corner of the screen.
- For each card, say the word out loud and try to say what you think the definition is.
- Flip the card by clicking on it and say the definition listed out loud.
Evaluation: Your lab performance will be evaluated by the criteria (standards) you will find in this project’s rubric. A rubric is simply a table that states how you will be evaluated. Your coach will use this table to report your performance.
CLICK HERE TO GO TO THE RUBRIC
_______________________________________
INTRODUCTION
Why does shocking someone stop cardiac arrest?
Interesting Facts to Know
Structure of the Heart
We all know that the heart is one of the most important organs in the body. While the lungs take in air so that oxygen can get into the blood, this would be useless without the heart. The heart is basically a pump that transports blood through the body. This allows both oxygen and nutrients to be delivered to the cells, while also taking away waste products such as carbon dioxide.
The heart is mostly made up of a special type of muscle called cardiac muscle, and has four major chambers. The upper two chambers are called the atria (AY-tree-uh), which is plural. The word for a single one of these chambers is atrium (AY-tree-um). The heart has a right atrium and left atrium. The lower two chambers are called the ventricles (VEN-trick-uhls). The heart has a right ventricle and a left ventricle.
 |
One thing to remember is that when we look at pictures of the body or its organs, they are usually drawn as if the person is facing us. So their right is on our left, and their left is on our right. This is common when talking about anatomy. You can see this in the picture of the heart shown here. |
| Muscular walls called septa (SEP-tuh), separate the left and right chambers of the heart. The word for just one of these walls is septum. On the other hand, the top and bottom chambers are separated from each other by one-way valves, which are white structures made of connective tissue. These are flaps that open and close only in one direction, to keep blood flowing on the desired path. For example, blood always flows from the atrium to the ventricle on both sides of the heart. So these valves open downward into the ventricles, and then close to become flat. This prevents blood from flowing out of the ventricles and back up into the atria. There are also valves between the ventricles and the giant blood vessels that they pump blood through. |
 |
Blood Flow through the Heart
The blood vessels of the body, the blood, and the heart, make up the circulatory (SER-cue-luh-tor-e) system. Blood flow through the circulatory system follows a one way path that must be followed to allow the body to function correctly. Let’s follow the blood through this entire system. Look at the picture which is numbered with each step:
 |
|
- Next the muscle of the two ventricles contracts, pushing blood up and out of the heart and into the vessels. The blood we are following now enters a giant vessel (shown in blue) called the pulmonary trunk, which branches off into the right and left pulmonary arteries (PUHL-mon-air-ee AR-tur-ees).
- The blood in the pulmonary arteries is pushed all the way to the left and right lungs, where oxygen enters the blood and carbon dioxide leaves the blood.
- After completing its journey through the lungs, blood is high in oxygen and has more of a bright red color. It comes back to the heart through the left and right pulmonary veins (PUHL-mon-air-ee VAYNS).
- The left and right pulmonary veins empty into the left atrium.
- The muscle of the two atria contract again, which is the beginning of a new heart beat. However the blood we are following just now enters the left ventricle.
- Next the muscle of the two ventricles contracts again, pushing blood up and out of the heart and into the vessels. The blood we are following now enters a giant vessel (shown in red) called the aorta (ay-OR-tuh).
- The aorta branches off into many more arteries (vessels that carry blood away from the heart) that carry blood to the upper and lower body, where oxygen and nutrients are delivered to the cells.
- Once oxygen and nutrients are delivered to the cells, and the blood has picked up carbon dioxide and other waste products, it is carried back to the heart through veins (vessels that carry blood towards the heart). All veins eventually empty into the two venae cavae, which then empty back into the right atrium. Then the cycle begins again!
*Notice that it actually takes two full heart contractions (or heart beats) for blood to pass through all four chambers of the heart.
To see all of these steps in action, check out this video:
(Don’t worry about the names of the valves, which we won’t cover in this lab. Just remember there are four valves: the ones between the atria and ventricles, and the ones between the ventricles and vessels they pump into.)
Coronary Circulation
 |
The heart needs love too! A lot of people may not realize it, but the heart cells need blood pumped to them just like all other cells of the body. Blood passing through it with each beat does not supply the heart cells with the oxygen or nutrients they need to function. That is why there are actually tiny arteries that branch right off of the aorta and supply blood to the heart. These arteries and the veins that carry blood away from the heart cells make up the coronary circulation (CORE-uh-nare-ee ser-cue-LAY-shun). |
Ever wondered why everyone says fatty foods cause heart disease and eventually heart attacks? It’s actually because high levels of cholesterol and certain types of fats can play a role in a person developing atherosclerosis (ath-ur-o-sclare-O-sis), meaning “hardening of a fatty substance in the arteries.” This hardening is due to the buildup of a plaque made up of cholesterol and fats, and this plaque makes the space in the vessels much smaller. This makes it much harder for blood to flow through the arteries.
When someone has a heart attack, also called a myocardial infarction (MY-o-car- dee-uhl in-FARK-shun), it is because a piece of this plaque or a small blood clot has lodged itself in one of the coronary arteries. This cuts off blood flow to a certain part of the heart, and when the tissue cannot get oxygen or nutrients from the blood, it begins to die. This requires immediate medical attention or the person’s heart may stop pumping blood successfully and eventually stop beating at all. This is called asystole (ay-SIS-toll-ee). You probably recognize this from movies where a person’s heart monitor suddenly flat lines, and the person dies.
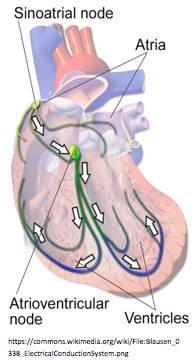
| How does the heart know when to pump? There is actually a network of electrical fibers in the heart muscle that causes it to contract. Perhaps the most important part of this network is where the signal starts, in a bundle of electrical cells called the sinoatrial node (sy-no-AY-tree-uhl NODE), often abbreviated as just the SA node. The SA node is located in the upper wall of the right atrium. Believe it or not, the SA node actually fires electrical signals on its own, without the brain telling it to! The brain only changes the speed of the heart rate or causes the heart to contract with more force. For this reason, the SA node is often called the “pacemaker” of the heart, because it sets the resting heart rate. |
 |
Electrical Activity in the Heart
Once a signal is fired from the SA node, it travels through fibers surrounding both atria and causes them to contract from top to bottom, pushing the blood down into the ventricles. The signal is also transferred to the atrioventricular node (ay-tree-o-ven-TRICK-you-lur node), often just called the AV node.
The AV node does not fire right away though. It shortly delays the signal, so that the atria can completely empty of blood before the ventricles contract. Then the AV node passes the signal to a bundle of fibers called the Bundle of His (pronounced “hiss”), which splits into two branches of fibers that run down the septum of the heart, called the left and right bundle branches.
The bundle branches go all the way down to the base of the heart, and then run outward and back up the sides of the heart through the purkinje fibers (per-KIN-jee FY-burs). These fibers deliver the electrical signal to the cells of the ventricles from the bottom upwards, causing the ventricles to contract from bottom to top. This forces the blood to be pumped upwards and into the giant vessels at the top of the heart.
This pathway of electrical activity is what you are actually seeing if you have ever seen the waves on a heart monitor! A heart monitor produces an electrocardiogram (ee-LECK-tro-CAR-dee-o-gram), or graph of the heart’s electrical activity, sometimes abbreviated as an ECG or EKG.
Check out this animation to see the heart’s electrical system in action:
https://www.nhlbi.nih.gov/health/health-topics/topics/hhw/electrical
Heart Rhythms
 |
As you may have noticed on the video, a healthy heart produces a series of repeating waves on an ECG. This normal rhythm is called a sinus rhythm. There are three main parts of the signal produced by a single heartbeat: the P wave, the QRS wave, and the T wave. |
Many abnormal heart rhythms exist, and skilled medical professionals are able to diagnose specific problems with the heart based on different patterns they see on an ECG. Today we will focus on two of the most common rhythms that can be experienced by victims of a heart attack.
When the flow of blood is blocked on its way to the heart during a heart attack, this often leads to failure of the heart's electrical system. The damaged electrical tissue in the blocked section can cause the rhythm of the entire heart to be thrown into useless patterns of electrical activity called sudden cardiac arrest, or failure of the heart to pump blood properly. This is NOT necessarily the same as asystole, or lack of any electrical activity and contraction. In fact, the heart muscle usually is still contracting, but it is disorganized and does not allow the proper filling and emptying of heart chambers. This means blood and therefore oxygen is not being delivered to the body, and death can result in minutes.
There are two extremely common rhythms that occur during sudden cardiac arrest. Neither rhythm produces a pulse that you can actually feel when someone attempts a pulse check, as described below.
Ventricular Tachycardia (ven-TRICK-you-lur tack-i-CAR-dee-uh), often just called V-tach, is an extremely fast beating of the heart that is caused by abnormal electrical signals that start in the ventricles rather than the atria. The ventricles beat at a consistent rate, but contract so fast that they do not have time to fill with blood.
While some blood may still get pumped out of the heart, it is nowhere near enough to keep the body functioning correctly. V-tach can also easily turn into the next rhythm, described below.
Ventricular fibrillation (ven-TRICK-you-lur fib-rill-AY-shun), often just called V-fib, is the more dangerous of the two because it can decline into asystole if not treated quickly. On an ECG this looks like a bunch of crazy, irregular peaks and dips that are constantly changing shape. These disorganized electrical signals cause the heart to simply “quiver” or shake uselessly, and blood flow to the body stops.

CPR

You’ve likely heard of CPR, and maybe you even know how to do it. CPR stands for Cardiopulmonary Resuscitation (CAR-dee-o-PUHL-mon-air-ee ree-SUS-it-AY-shun). If you’ve never seen it in real life, you’ve probably seen it in the movies (although probably not done well!) There are two main parts to CPR: chest compressions and rescue breathing.
Chest compressions are meant to restore blood flow in the victim. It has been shown that compressing the heart repeatedly can force it to push a decent amount of blood through the body as if it were pumping on its own (although of course not as effective as a functioning heart). This keeps the brain and body alive because there is still oxygen in the blood that has not been used by the tissues yet, so getting the blood moving provides a small amount of oxygen to the cells.
Rescue breathing is meant to supply the victim with more oxygen that can be transferred to the blood through the lungs, and then pushed through the body using chest compressions. While many people may think that the air we breathe out is low in oxygen (we already used it up ourselves, right?) this is actually not true. In fact, the air that we breathe in is about 21% oxygen, but the air we breathe out is still about 14-16% oxygen! So when we give someone a breath using our own exhaled air, it is still quite full of oxygen!
Hands Only CPR
The American Heart Association has come to recognize that one of the main reasons people fail to give CPR is because most people are extremely uncomfortable with the idea of giving “mouth to mouth” to a stranger. For that reason, “Hands Only CPR” was developed, and in many studies it was actually found to be nearly as effective as regular CPR for the first few minutes after cardiac arrest! This can really be the difference between life and death for a victim, because without CPR the brain is not getting any oxygen at all, and after only 6 minutes that person will likely have permanent brain damage. After 15 minutes, almost no one survives. Providing CPR, even Hands Only CPR, can extend a person’s time and increase their chance of survival by getting oxygen to the body until help arrives.
 |
When you find someone who is unconscious, not breathing and who has no pulse, CPR should be started right away. There are only two steps to Hands Only CPR:
|
But how fast is 100 compressions per minute? Check out this video to learn a great memory tool that will help you reach this goal if you ever need to use Hands Only CPR:
Full CPR
Of course if you know the person who needs CPR, you would probably be less hesitant to give mouth-to-mouth. Performing full CPR is actually not much more complicated than Hands Only CPR! We just need to add a couple more steps:
- Call 9-1-1.
- Perform 30 HARD and fast chest compressions in the middle of the chest, at a rate of at least 100 compressions per minute (remember…Stayin’ Alive!)
|
 |
An easy way to remember these steps is “C-A-B”: Compressions-Airway-Breathing
Full CPR can even be safely done on a stranger if you are prepared by having a face shield, which is a plastic barrier that has a one-way valve in it. This goes over the person’s face, with the valve lined up over their mouth. The valve allows you to blow through it into their mouth, but prevents anything from coming back through to your side. These are great tools that can really improve the quality of CPR, and many companies even sell them in pouches that you can attach to your keychain!
Defibrillation
How many times have you seen a TV show or movie, where someone is in the hospital, the person’s heart rate suddenly flat lines, and the doctor shocks them to bring them back to life? It makes for a great dramatic ending, but too bad that it’s completely false.
Asystole (lack of electrical activity) is never a “shockable rhythm,” even for doctors. This is because delivering a shock to the heart, called defibrillation (dee-fib-rill-AY-shun), is designed to act as a “reset button.” During cardiac arrest, the heart’s electrical system is out of whack. The shock is a way to stimulate the SA node to start firing normally again. When a person is in asystole, there is no electrical activity to reset. In real life, no one ever shocks a flat line.
In fact, the two rhythms that usually are shocked are V-tach and V-fib, the rhythms discussed earlier. Both of these rhythms are quite likely to be “reset” with the appropriate electrical shock. In fact, this treatment has become so well accepted that Automated External Defibrillators (AEDs) were created to allow any untrained person to use them. This is a machine that when turned on, talks and tells a person exactly which steps to take in order to deliver a shock to a person in cardiac arrest. It has two pads that even have pictures of where to place them on the person.

Unless you SAW the person collapse, it is recommended to give at least 2 minutes of CPR before a shock is delivered. If performing full CPR, this is 5 cycles of the 30:2 ratio. It will then say to “clear the patient,” meaning to make sure no one is touching the person. The AED will “analyze” the person’s heart rhythm and figure out if they are in V-tach or V-fib, the only two “shockable rhythms.” If so, it will give instructions to deliver a shock. If not, it will advise you to keep performing CPR.
AEDs have become so easy to use that you may actually see them in malls, airports, grocery stores, and many other public places all over the world. They will usually have one of several types of signs above them like one of the pictures you see here. You really need no training to use them; you just have to be willing to try it when you see someone in need!



__________________________________________
Links to Station 4.2 Modules
Lab Intro | Lab Presentation and Practice | Communications Intro| Communications Presentation and Practice| Math
